(and the rational doctor).
There is no disputing the fact that the pressure on the open doors of the NHS – primary care, urgent and emergency care – is unmanageable. One recurring cry from GPs and A&E staff is that they are seeing ‘the wrong people’ – that one patient takes up a GP appointment with a ‘trivial problem’ while another fails to get an appointment and becomes an emergency, or at least accesses unscheduled care, as a result. In addition, A&E waiting times are at least in part being affected by the need to triage and see patients who don’t need the specialist services of an emergency department (though this is not the main problem).
Recent NHS England campaigns illustrate the difficulty of trying to modify health-care seeking behaviour that has risk-judgement at its core.
On the one hand we have campaigns such as Choose Well (or as I call it – Don’t bother the busy Doctor), clearly aimed at over-consulters. The various configurations of these posters and websites attempt to categorise services by symptom, but ‘tummy ache’ could be period pain or pancreatitis – and most advise you to consult your GP if your symptoms don’t go away, without specifying how long the course is likely to be. For a cough, 3 weeks is normal, but I doubt most GPs would want a patient with a severe headache to wait more than a couple of days.
On the other hand we have the “Minor Illnesses can get worse quickly in the Over 60s” campaign, which seems to target under-consulting, but has a deep incoherence. The smaller print on the posters directs people to consult their pharmacist, but most of the products that a pharmacist can supply for minor illnesses target symptoms, not causes, and cough mixtures and paracetamol will not halt your infection – though simple self-care such as keeping warm and hydrated might give your own immune system a better chance. Presumably the pharmacist’s role in preventing escalation here is mostly as triage, but in a ring-at-8am-and-cross-your-fingers same day appointment system, directing someone who might deteriorate quickly to try the pharmacy first is only likely to delay the useful consultation with a GP who can give steroids, antibiotics and so on. If it doesn’t delay consultation then that is because the GP is willing to tag emergency patients on to their later sessions when the patient presents at 3pm because the pharmacist has told them they need a consultation today.
The biggest weakness of both campaigns is that they’re trying to nudge behaviour that is too complex to be nudged by such simple messages.
Nudging the normal curve is challenging
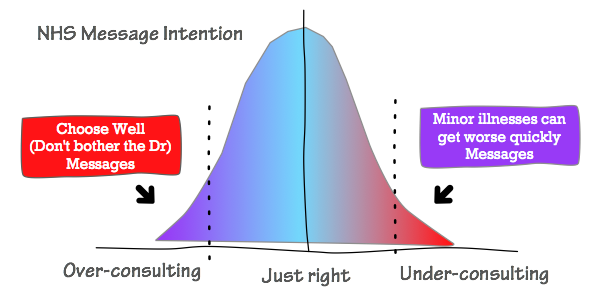
Let’s make a crude assumption that the population’s risk-threshold for consultation is roughly normally distributed, with the average behaviour being appropriate consultation. Under-consulters and over-consulters lie at either side of the curve.
The Choose Well campaign is attempting to nudge over-consulters towards the average (just right) behaviour. The Over-60s-get-ill-quickly campaign is trying to nudge under-consulters towards the average. As a combined strategy, they are attempting to narrow the curve, to push more people towards ideal, “appropriate” consulting behaviour. They want to nudge the curve until it looks like this:
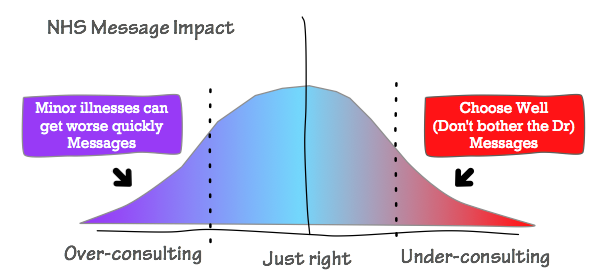
It’s an excellent intention. Narrowing the curve would result in fewer ‘wasted’ appointments and fewer ‘avoidable’ escalations. Unfortunately this is not how human behaviour works. All people are affected by confirmation bias – we are more attuned to, and more likely to put weight on, signals and messages which confirm the beliefs and thoughts that we already have. This means that the over-consulters are highly attuned to the ‘Get worse quickly’ message, and the under-consulters are very sensitive to the “Choose Well (Don’t bother your doctor)” message. Instead of having impact as intended, the signals cross over, and the impact on the consulting-curve is more like this:
It’s actually even harder – there isn’t one curve, there are many curves
The majority of people are located in a different place on the consulting curve depending on the condition, symptoms and situation. A parent may be a serial under-consulter themselves but an over-consulter for their child. A person might under-consult for their migraines, missing their treatable high blood pressure, but over-consult for a case of blepharitis (icky eyelids) because their appearance matters to them a great deal. A ‘sore knee’ that is no big deal to a receptionist might be a major problem for a farmer or window cleaner. Mild-chest-discomfort might be terrifying for someone who lost a parent to an early heart attack.
I was fortunate not to lose my Dad early, but knew that he had heart problems from his 30s onwards, and he is only here today because he survived an emergency triple bypass at 50. His first episode was while running in Hyde Park – fortunately his running buddy was the company GP. So when my heart rate monitor told me I’d had an average of 200 and a peak (sustained) heart rate of 217 on a run recently, the intense burning in my chest I’d had afterwards took on a sinister tinge. I visited Dr Google, debunked the 220-age maximum-rate limit, read that the athletes-have-a-low-heart-rate story is a myth, reassured myself that the more important thing was that my heart rate recovered rapidly when I stopped running, reminded myself that I’d just started a new medication that could affect electrolytes, and still went to bed scared. I was lucky that I had an appointment and bloods booked because of the new medication, and that my GP is not the one-thing-per-appointment type, so we were able to discuss it. She was reassuring. I’ve since discovered that it only happens in very cold weather (new PB is 218 BPM) – so all is well. If my own GP had been on holiday, I might have been a “patient consulted because their heart beats fast when they run… duh!” anecdote.
Some patients may not disclose their ‘real’ reason for consulting because they don’t want to put ideas in the doctor’s head – they want to see whether their doctor mentions ‘heart’ before they mention it themselves. They may get home and say to their spouse ‘See – I knew I was being silly… he never even mentioned cancer!’
You can do excellent ICE but you will never have the full picture – the patient may not even be able to articulate the reason why they came, and if they can, the idea that if only we could teach people the ‘rules’ for appropriate consulting then half our problems would be solved largely misses the reality of human decision making. Most of our thinking is twisted and polluted by bias, heuristics (short cuts for making decisions) and fallacies. And when I say “our”, I mean all of us, doctors and nurses as well as patients.
Special case fallacy
HCPs may know the current best evidence basis for a particular presentation, for example the Ottawa Ankle Rules for determining whether to x-ray an injured ankle. One of the indicators (in the absence of other specific findings) is whether the patient is able to weight bear for four steps. The rules are very specific – four steps. But the Doctor may still send a patient who can bear weight for five or six steps, or more steps with significant wincing, for x-rays. Their justification is that this patient is a ‘special case’. The rules are 98.5% sensitive, so there should be very few ‘special cases’ out there, and most are probably people with undiagnosed bone weaknesses, but doctors tend to pick out special cases for more human reasons “He’s a rugby player – hard lad.”
Patients can also be taught the Ottawa rules, but they make little or no difference to how frequently they present to the ED. Patients either fear that they aren’t quite applicable in their case (special circumstances) or that they will be in the 1-in-50 (maximum – most studies found it to be less than this) who are the special cases.
The same applies to URTIs. Most coughs and sinus infections clear up on their own, but it is a fact that some don’t. Patients do suffer bacterial chest infections, burst ear drums, pneumonia, and most patients are aware that these are potential hazards.
Doctors are attempting to address this by teaching patients the equivalent of the Ottawa rules for URTI, but this has the potential to dilute the value of the history in diagnosis. If patients know that they should wait 3 weeks before consulting for a cough, guess how many more patients will claim that they’ve had their cough for 3 weeks when you see them? Patients may present a day or two later than they would have, but instead of reducing treatment of self-limiting illnesses, we are likely to see increased treatment due to the ‘adapted’ history required to justify consulting the doctor.
Patients aren’t being Bad in doing this – they believe themselves to be the special cases, they fear the consequences of delaying treatment (or they need to consult you to be allowed entry to the sick role in their family or workplace). I’ve no doubt that the parents who consulted Jonny Tomlinson over the New Year were genuinely very worried by their babies’ breathing:
if every single mother of a child with a cold tells me they have rapid shallow breathing today, it’s one less useful bit of history
— Jonathon Tomlinson (@mellojonny) January 1, 2015
The Gambler’s Fallacy
The gambler’s fallacy causes people to believe that if they have tossed a fair coin 5 times and it has come up tails 5 times, the next flip is almost certain to come up heads.
When I was 14 I had increasingly horrible abdominal pains. The pain started just above my right hip and then then moved to the middle. But my mum knew that it couldn’t be appendicitis because my friend Katie had just had appendicitis two weeks ago, and the chances of us both having it were very small. So we presented late, via the GP who seemed puzzled and concerned that my mother had delayed consulting about such a textbook presentation of appendicitis when she definitely knew the symptoms – my sister had had suspected (ruled out) appendicitis before. Several hours later I was minus my appendix, which turned out to be both disgusting and not systemically linked to that of my friend.
Attribute substitution
In this bias, we substitute a simple decision for a highly complex one – at least consciously in our explanation. A GP may make a decision to give antibiotics for a child’s cough because of a complex constellation of risk factors and subtle signs in the history (including that of the wider family), and the examination. The GP develops a gut feeling that this one is worth treating. Understandably, the explanation given to the parent is a simpler one “We don’t normally give antibiotics for coughs in children, but I really don’t like the sound of this one…” (no clarity about whether this is the pronounced bark or the lung sounds heard via stethoscope) “… and he’s obviously very tired.”
Mum goes home and repeats this explanation to the parents of Jimmy’s best friend, who has a similar sounding cough and is also tired by poor sleep, and now they believe that he also needs antibiotics and are furious (with genuine fear for their child) when they are refused them by their own GP.
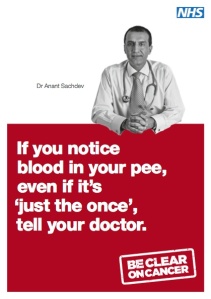
Attribute substitution is the mechanism behind red flags and NEWS scores. Based on evidence, we gather highly sensitive and/or specific signals and set them up as shortcuts to decisions. In the context of expertise, the expert, perhaps an experienced GP, can also rapidly assess whether this case is an exception. When we rely on attribute substitution for non-expert triage, as in the 111 service or the ‘If you have blood in your pee, even just the once…’ bladder cancer campaign, the result is typically over-estimation of risk.
Attribute substitution also results in significant under-diagnosis. “We didn’t consider Addison’s because you had normal potassium” missed the fact that a third of patients with addison’s don’t have elevated potassium at diagnosis and patients who are taking a lot of beta-agonists (because their asthma is uncontrolled due to low cortisol) typically have low potassium – so a ‘normal’ potassium is an unexpected finding. The attribute substitution of ‘High potassium – think Addison’s’ drowns out the fuller picture of a complex diagnosis. Parents and teachers who say “If you can wiggle your fingers your wrist can’t be broken” delay presenting their children with upper limb fractures. Substituting a single sign for a complete picture is both useful and dangerous.
Magical thinking – conditional
- “I’m lighting a fag to make the bus come.”
- “If I don’t take my umbrella it is bound to rain.”
- “These things always happen when we’re going on holiday!”
People have beliefs that they can ward off an unwanted event by preparing for it – they genuinely believe that if they pick up a script for antibiotics ‘just in case’ then they are less likely to get a serious infection.
I hear HCPs use the same wonky logic – If I don’t get an x-ray of this person’s ankle who can walk 5 steps, it’s going to be the fracture that I miss this week. If I don’t do the TFT on this patient who is Tired All The Time they will turn out to be the one in a bzillion who is hypothyroid. Poked hard enough, doctors reveal beliefs that their tests alter the prognosis for the patient, not just their treatments.
Magical thinking – superstitious
“Bad things happen in threes, and I’ve already had two this week.”
“My horoscope said Thursday was going to be an unlucky day for me (so this pain I have is bound to be something serious).”
“I prayed about his chest pain and then when I fell asleep I had a dream that my husband was dying but the paramedic saved him.”
I grew up in a very religious (evangelical Baptist) home, and am now an atheist. Despite my feeling that they just have a very popular imaginary friend, I can’t deny that to many people who I respect, the guidance they feel they receive from their God/s is very real. They may interpret ‘signs’ as being extra meaningful – “There was a patient with a PE on Casualty this week and then I woke up with a pain in my calf – Jesus is really looking after me…” Without getting into any deeper comment about the pros and cons of religion, this is – at worst – simply another cognitive bias among so many others, but one that is particularly likely to be hidden in the healthcare setting (though perhaps spoken about vigorously in the church).
Identifiable victim effect
We tolerate risk differently when the potential harm is going to happen to somebody who we can identify. Although the impact is greatest when it involves people we are close to, we don’t have to have a deep relationship with the victim, just for them to be differentiated from total-strangers.
You can see this if you watch twitter conversations between HCPs for a little while. The ‘can’t be too careful’ messages emerge when we’re considering the possibility of serious illness in someone who we have a twitter relationship with, even if we might express the opposite message about the same symptoms in the general public. We justify this as being because we know certain details about this identifiable specific person. Yet we have no information to frame the unknown people who we feel should take a different decision, who may also be known to be sensible, stoic, etc – but of course only by people who know them.
Availability heuristic
The tendency to overestimate the likelihood of events with greater “availability” in memory, which can be influenced by how recent the memories are or how unusual or emotionally charged they may be.
I believe this is one of the most important factors that makes designing successful ‘nudge’ public information campaigns so difficult. Unusual things stick in our minds, and dominate our media. Magazines are filled with one-in-a-million stories – tragic cases of that-lump-on-my-finger-was-malignant. You can present 1000 cases of self-limiting viral illness and one of meningitis and inevitably the tragic and serious one is the story that sticks. We simultaneously want to ‘raise awareness’ of under-diagnosed serious conditions, and expect people to understand that most illnesses are unimportant and not dangerous. If human beings were able to manage this kind of statistical information no lottery tickets would be sold. 70% of UK Adults regularly buy a lottery ticket.
There are many other interesting cognitive biases and judgement heuristics – far too many to explore here. The fact that educated, intelligent and self-aware HCPs also struggle with bias in their decision making should caution against the idea that patients ‘just need to use more common sense’.
Until we better understand why people are consulting, and the role of the promotion of preventative medicine for ‘invisible illnesses’ in reducing the threshold at which all people consult (not just those on preventative treatments), we’re doomed to produce crude information campaigns that cost money and don’t produce results. I don’t know what the answer is, but spending money on things that clearly aren’t answers is definitely not useful. Total Triage is one strategy (with mixed results), but I personally fear that I wouldn’t have had the relationship with my GP that has been so crucial in having long term illnesses if I hadn’t met her twice when I was ‘well’ with acute, non-serious problems.
Of course the other unspoken factor in pressure on the doorways to health care is that there has been a rapid increase in survival. We just aren’t dying very efficiently any more.
Reduced ‘tolerance’ of illness is a symptom of the success of medicine
There seems to be a public yearning for the good old days, when people knew how to be sick in the quiet of their own homes and didn’t whinge about coughs and colds.
A golden age of poultices, when most families could expect to lose a child to illness. When measles, mumps and rubella killed and maimed without people making such a fuss and the press putting it on the front page.
If you were, like me, born before 1980 then the chances are that you had most, or a full house, of the serious illnesses of childhood: measles, mumps, chicken pox. You probably had a couple of severe bouts of flu, because pre-vaccination it spread much more successfully, and maybe some of the wildfire diseases like parvovirus and whooping cough.
Today, most children reach adulthood without the same CV of infectious diseases survived. They have fewer experiences, and their parents have fewer experiences, of surviving a raging fever that lasts more than a few days. And that is a good thing, and we shouldn’t judge them for having an illness-threshold that is calibrated to coughs and colds and hangovers.
They’re not more selfish, they are less experienced – because we collectively decided to take those experiences away from them, in order to spare the ones who die or are disabled by the conditions we now vaccinate against.
—
Refs:
http://en.wikipedia.org/wiki/List_of_cognitive_biases
http://en.wikipedia.org/wiki/Heuristics_in_judgment_and_decision-making
Over 60 – Minor illnesses get worse quickly campaign
http://www.choosewellwales.org.uk/home
http://www.nhs.uk/be-clear-on-cancer/assets/BeClearOnCancer_BloodInPee_leaflet.pdf
Primary care telephone triage does not save money or reduce practice workload

Reblogged this on Mental Health Geek.
Pingback: Resilient GP: an ethically inappropriate survey report | jonmendel
fabulous piece of writing. will use as reflective piece for teaching registrars/medical students in family medicine.